Current Issue
Necrotizing Fasciitis and Diabetic Ketoacidotic: A Potentially Fatal Combainaison
Nassima Dekdouk1,*, Rachid Belhadj1, Khadidja Benmahieddine1, Habiba Berrouane2, Charafa Zine Amir2
1Forensic service, "penitentiary unit", Algiers, Algeria
2Department of Anatomopathology, Mustapha Hospital, Algiers, Algeria
*Corresponding Author: Nassima Dekdouk, Forensic service, "penitentiary unit", Algiers, Algeria; Email: [email protected]
Received Date: February 26, 2024
Publication Date: March 20, 2024
Citation: Dekdouk N, et al. (2024). Necrotizing Fasciitis and Diabetic Ketoacidotic: A Potentially Fatal Combainaison. Diab Res. 1(1):2.
Copyright: Dekdouk N, et al. © (2024).
ABSTRACT
Necrotizing fasciitis is historically described as a “flesh-eating bacteria” and is a life-threatening emergency. Unusual presentations can blind clinicians. Prompt diagnosis and treatment can make the difference between life and death. These infections occur more frequently in diabetics and are associated with higher morbidity and mortality rate. The predisposing factors are diabetes mellitus, immune compromised state, other metabolic disorders and vascular insufficiency.
Diabetic acute complication, diabetic ketoacidosis is an extreme and fatal metabolic state of uncontrolled diabetes. It has been shown to cause metabolic acidosis, drowsiness, and shock in patients, and infection is one of the most common causes of diabetic ketoacidosis.
This is a report of a case Necrotizing fasciitis in a patient complicated with diabetic ketoacidosis it’s about a 63-year old man patient who presented with many risk factors favoring the occurrence of necrotizing fasciitis, namely diabetes mellitus, heart failure chronic renal failure and obesity. Despite treatment; the patient then succumbed.
Its rarity and the paucity of early pathognomonic signs make Necrotizing fasciitis a major diagnostic challenge. The differentiation of necrotizing fasciitis from other soft tissue infections is therefore critically important.
Keywords: Necrotizing fasciitis, diabetic ketoacidosis, diagnostic challenge, Fatal combainaison
INTRODUCTION
Necrotizing Fasciitis (NF) is a rare, rapidly progressive infectious process primarily involving the fascia and the subcutaneous tissue, with thrombosis of the cutaneous microcirculation. The propagation velocity is directly proportional to the thickness of the subcutaneous layer. Necrotizing fasciitis travels around the plane of the fascia [1]. Despite the severity of the disease, the diagnosis of NF can be difficult with the diagnosis being missed in 85% to 100% of patients [2].
This disease develops rapidly, such that clinically, early recognition and timely surgical incision and drainage decompression are needed, otherwise it can readily lead to multiple organ failure and septic shock, even becoming life-threatening, with mortality rate as high as 25–35% [3,4].
Diabetes mellitus is one of the serious conditions, associated with necrotizing fasciitis. It is a disorder that primarily affects the microvascular circulation. In the extremities, microvascular disease, due to sugar-coated capillaries Q limits the blood supply to the superficial and deep structures [5].
Diabetic ketoacidosis (DKA) is another serious complication of diabetes, which can occur when the body does not have enough insulin to break down glucose for energy. This causes the body to start breaking down fat for energy instead, leading to various complications.
CASE REPORT
A 62-year-old man who presented at the hospital difficulty breathing when lying down wheezing, coughing, fever swelling in the lower part of the body. With high fever, chills, and severe pain at the of his right leg.
Her medical history was significant for type 2 diabetes for the past 5 years, class 2 obesity (body mass index 37.5 kg/m 2), and hypertension for the past 10 years. Mechanical aortic valve replacement under anticoagulants; heart failure, kidney failure, sleep apnea syndrome (SAS).
On admission, the patient exhibited signs and symptoms of DKA, including hyperglycemia, metabolic acidosis, and ketonuria. The Glasgow Coma Scale (GCS) score of E3V4M6, indicating impaired consciousness, along with a blood pressure reading of 140/60 mmHg, was febrile (temperature 40°C), tachypneic (respiratory rate 20), tachycardic (heart rate 120).
Physical examination revealed an Erythema and extreme swelling, redness of the skin, warmth swelling tenderness in an area of skin leaking of yellow clear fluid or pus. And the congestive heart failure (acute pulmonary edema).
Admission laboratory studies revealed blood sugar levels exceeding 600 mg/dl, the presence of 4+ urinary ketone bodies; Hb 10 gm % 13-17 gm % TLC 40400 cells/cu mm (4000-10000 cells/cu mm) Platelets 2.57 Lakhs/cu mm (1.5-4.1 Lakhs/cu mm) Urea 60 mg/dL (19-43mg/dL) Creatinine 4.5 mg/dL(0.66-1.25 mg/dL) c –reactive protein (CRP) blood test 300 mg/L (less than 5 mg/L).
Sodium 137 mmol/L (137-145 mmol/L) Potassium 3.5 mmol/L (3.5-5.1 mmol/L).
Emergency Ultrasound Eliminated a Vein Thrombosis
An orthopedic consultation was obtained and an initial diagnosis of cellulitis was made (figure 1). The patient received prompt and appropriate management, including adequate hydration, intravenous antibiotics (cefotaxim, metronidazole), treatment of the heart failure and insulin therapy to correct the ketoacidosis.
However, his fever did not subside, despite the administration of intravenous antibiotics. Her erythema and bullae worsened (Figure 2); on day 5 of admission, a decision for surgical exploration was made to exclude NF. A sample of tissue was sent for histologic assessment.
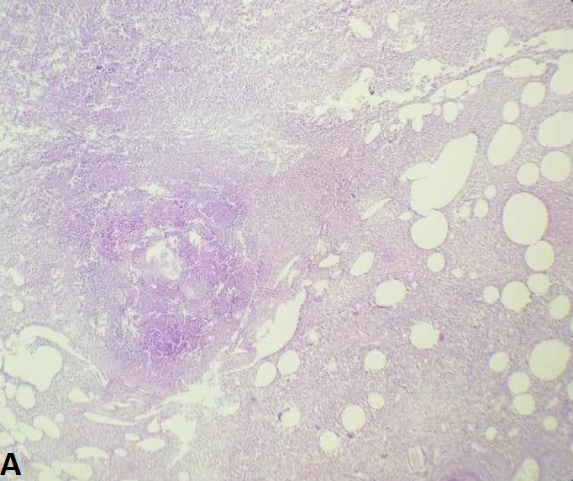
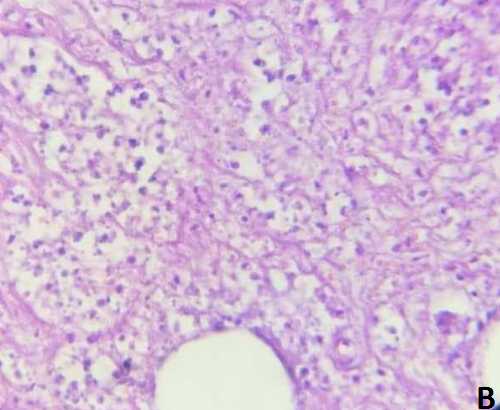
Histology results were reported as consistent with NF (Figure 3). Cultures obtained from the debrided tissue confirmed the presence of a polymicrobial infection (Extended-Spectrum (Escherichia coli Beta-Lactamase (ESBL) Producing positive), pseudomonas spp, Proteus spp.
Broad-spectrum antibiotics were initiated (Imipenem, Ciprofloxacin) targeting the identified pathogens.
With the diagnosis established, NF; the patient was immediately taken to the operating room for incision and debridement.
Given the low immunity determined by heart failure, obesity, kidney failure and decompensated diabetes mellitus, the general condition of the patient quickly worsened, with the decrease in plasma levels of hemoglobin and albumin, with hydro-electrolytic imbalances, metabolic acidosis etc., which could not be compensated despite all the efforts. The patient died 2 weeks after the onset of the necrotizing fasciitis.
Figure 1: Initial diagnosis “cellulitis”
Figure 2: Rapidly progressive skin lesions had developed on both lower extremities (erythema and bullae worsened)
Figure 3: Photomicrograph of histopathological specimen at low power (4X) (A) and Higher power (40) (B) examination demonstrates impressive suppuration and extensive tissue necrosis.
DISCUSSION
Necrotizing fasciitis was first mentioned by Hippocrates around the fifth century ad as a complication of erysipelas. Joseph Jones in 1881, provided one of the earliest description of this clinical entity and named it hospital gangrene [6-8]. In the year 1924, following a study of 20 patients in China Meleney made the discovery that the etiological agent responsible for this particular pathological condition is hemolytic streptococcus. [5,8-10]. The term necrotizing fasciitis, first coined by Wilson in 1952, is perhaps the most accurate for describing the key features of this infectious process [5,9,11,12].
The condition was classified as hemolytic streptococcal gangrene. However, in 1972, B. Wilson introduced a significant diagnostic indicator known as fascial necrosis. Hence, the widely acknowledged definition of necrotizing fasciitis, as proposed by B. Wilson, has been established [9].
Necrotizing fasciitis occurs at any age with a mean age variation from 32 to 57 years [8,12], with a slight male predominance [12-16].
There are multiple risk factors that may contribute to a higher incidence of NF, including chronic diseases; diabetes mellitus obesity cirrhosis malignancy renal failure acquired immune deficiency syndrome, gout, peripheral arterial occlusive disease, myelodysplastic syndrome;
Corticosteroid therapy and chronic traumatic smoking alcohol abusers intravenous drug use have been established [1,2,5,12,13,15,17-20].
Diabetes is the most important comorbidity of NF, accounting for 40% to 72.3% of the overall population of patients with NF [6,7,18,19,21,22]. However there was no significant difference in mortality between diabetic and non-diabetic patients, although it is often remarked that mortality is increased in the presence of diabetes mellitus, which is not always the case [20,21].
Diabetic patients are well known to be afflicted with foot problems caused by neuropathy and microvascular disease, which render limb preservation more difficult in the presence of a superimposed NF infection [3,19].
During infection, the endogenous production of glucose is increased from the overall increased rate of catabolism. Hyperglycemia has been found to affect adherence, chemotaxis, and bactericidal activities of phagocytes. On the other hand, hyperglycemia has been shown to have detrimental effects on cellular immunity [23].
The patients with necrotising fasciitis can present included pain at affected site fever and swelling and the most common signs included tenderness tachycardia erythema and induration The other notable clinical features included skin discoloration and bulla formation [4,12,17,24,25]. However, crepitus was not a common finding [17,24].
The diagnosis of NF can be rather difficult but should be considered in patients presenting with rapidly spreading erythema, pain and discolouration [25], the most commonly affected areas are the limbs and perineum [4,12,16]. Necrotizing fasciitis of the extremities is the most frequent clinical presentation [12,13,24].
The diagnosis must be made on clinical signs grounds and history (predisposing factors to infection). If the infection contains gas-forming agent, localised crepitus can be detected by plain radiographs or T2 -weighted magnetic resonance imaging (MRI) very sensitive in fat and ultrasonography can be helpful in diagnosis [5,26].
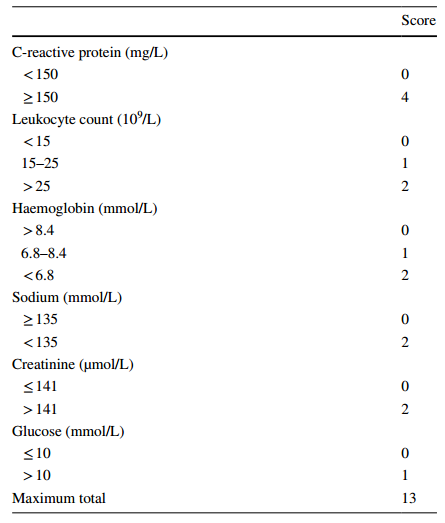
Early stages of disease are often misdiagnosed as cellulitis or abscess because of the absence of specific clinical features. Wong et al. described the “Laboratory Risk Indicator for Necrotizing Fasciitis” (LRINEC) score (12), which is based on routinely performed laboratory tests (table 1). Investigations readily available at most centres, that can help to distinguish necrotizing fasciitis from severe cellulitis or abscess [2,4,13,14,20,25,27].
An LRINEC >6 has been found to have a positive predictive value of 92% and an LRINEC <6 has a negative predictive value of 96% [2,12]; However, this is not a substitute for clinical judgement [28].
Tan et al. reported that patients with diabetes have a significantly elevated LRINEC score compared to their counterparts and demonstrated that a cutoff of 8 or greater was significantly more sensitive in patients with diabetes compared to patients without diabetes [2].
The severity of disease was dependent on the virulence of the organism and has been classified as : type I: Polymicrobial, where a mixed aerobic and anaerobic infection is the cause (which could be due to Acetinobacter baumanii and rarely Vibrio spp ; type II: Monomicrobial infection is due to Group A Streptococcus and occasionally methicillin resistant Staphylococcus aureus (MRSA) ; type III: Gas gangrene infections are most commonly caused by the anaerobe Clostridium perfringens [1,3,10,11,14,16,19,26,28,29] Type 4 is of fungal origin and it affects the immunocompromised and involves Candida species. However, type 3 and 4 are not as frequently encountered as type 1 and 2. [14]
Patients with diabetes generally present with polymicrobial type I disease; [22] E.coli was the most common bacterium isolated from necrotic tissue of diabetic patients [12,20].
Sharp et al. demonstrated that E. coli was one of the four common organisms isolated from type 1 necrotizing fasciitis patients [20].
Necrotizing fasciitis is a flesh-eating disease is highly lethal, early diagnosis, early and aggressive surgical debridement supported by appropriate antibiotic and correction of metabolic disorder were key to success [29].
As an empirical therapy, broad-spectrum antibiotic combinations against gram-negative, gram-positive bacilli and anaerobes should be used. Among the many choices are vancomycin, linezolid, or daptomycin combined with one of the following: either piperacillin-tazobactam or a carbapenem or ceftriaxone plus metronidazole, or a fluoroquinolone plus metronidazole [1].
Surgical treatment can vary from the simple debridement to the disarticulation of the limb.
In a retrospective review of 68 patients, Bilton et al reported 4.2% mortality for patients undergoing early surgical debridement and 38% mortality for those with delayed treatment [12].
Debridement into the tissues below the deep fascia is not indicated, except when external injury has penetrated this layer. Amputation is rarely indicated because of the superficial involvement [10].
However, if the causative operation is from the bone amputation is unavoidable.
Without prompt treatment with appropriate antibiotics and/or debridement of infected tissues, patients may develop toxic shock syndrome, leading to multiple organ failure and mortality [3].
Table 1: The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC score) [1,2,9,18,27].
Score <6: low risk of having necrotizing fasciitis; 6 - 7: intermediate risk; ? 8: high risk.
CONCLUSION
Necrotizing fasciitis (NF) is a severe soft tissue infection with a high morbidity and mortality. With early diagnosis and treatment this could be reduced. Unfortunately, the diagnosis of necrotizing fasciitis can be very difficult. In recent years many risk factors have been identified. Diabetes mellitus is a common comorbid disease associated with necrotizing fasciitis.
Control of DKA and aggressive surgical intervention may be key approaches in securing a positive prognosis. However, more explicit evidence and experience is needed to elucidate the most efficacious therapies for this combined condition.
REFERENCES
- Reshna V. (2021). Diabetes Mellitus: A Predisposing Factor of Necrotising Fasciitis. Int J Pharm Sci Rev Res. 69(1):48-50.
- DeGenova DT, Hyland SS, Peabody T, Schmitz NP, Myers D, Patterson R, et al. (2023). Differences Between Patients With Diabetes Mellitus and Those Without in Cases of Necrotizing Fasciitis. Cureus 15(3):e36576.
- Li X, Du Z, Tang Z, Wen Q, Cheng Q, Cui Y. (2022). Distribution and drug sensitivity of pathogenic bacteria in diabetic foot ulcer patients with necrotizing fasciitis at a diabetic foot center in China. BMC Infect Dis. 22:396.
- Chowdary MS, Srinivasan D, Sreeramulu PN, Tejaswini MP, Krishna Prasad K, et al. (2021). The clinical efficacy of laboratory risk indicator for necrotizing fasciitis score in early diagnosis of patients with necrotizing fasciitis. Int Surg J. 8(7):2133-2139.
- Gürlek A, Firat C, Oztürk AE, Alaybeyo?lu N, Fariz A, Aslan S. (2007). Management of necrotizing fasciitis in diabetic patients. J Diabetes Complications 21:265-271.
- Kim J, Yoo G, Lee T, Kim JH, Seo DM, Kim J. (2022). Classification Model for Diabetic Foot, Necrotizing Fasciitis, and Osteomyelitis. Biology. 11:1310.
- Goh T, Goh LG, Ang CH, Wong CH. (2014). Early diagnosis of necrotizing fasciitis. Br J Surg. 101:e119–e125
- Afifi RY, El-Hindawi AA. (2008). Acute necrotizing fasciitis in Egyptian patients: A case series. international journal of surgery 6 (2008):7–14.
- Matmurotov KJ, Parmanov SA, Atajanov T. (2020). Optimization of Diagnostic Criteria for Necrotisius Fasciitis in Diabetes Mellitus, Texas. J Med Sci. 23:70-74.
- Sadasivan J, Maroju NK, Balasubramaniam A. (2013). Necrotising fasciitis. Indian J Plastic Surg. 46(3):472-478.
- Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. (2003). Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am. 85(8):1454-1460.
- Vidhyarthy AK, Abhishek K. (2023). A prospective study on outcome of necrotising fasciitis in relation to clinical features and bacteriological pattern. Int J Acad Med Pharm. 5(3):379-382.
- Peetermans M, de Prost N, Eckmann C, Norrby-Teglund A, Skrede S, De Waele JJ. (2020). Necrotizing skin and soft-tissue infections in the intensive care unit. Clin Microbiol Infect. 26:8e17.
- Halbhavi SN, Reddy R, Kalburgi EB, Poulose A, Gowd YCV. (2018). Clinical and microbiological profile of necrotizing fasciitis. Int Surg J. 5(6):2119-2126.
- Kaur N, Mittal S, Kapoor S, Gupta A. (2021). The study of the prognostic outcome of necrotizing fasciitis patients with and without diabetes mellitus. Int Surg J. 8(2):563-568.
- Vishnoi V, Chiam HC, Liebenberg P. (2018). Necrotizing Fasciitis: A Review of Outcomes from Necrotizing Fasciitis in Regional Far North Queensland. J Trop Dis. 6: 285.
- Dworkin MS, Westercamp MD, Park L, McIntyre A. (2009).The epidemiology of necrotizing fasciitis including factors associated with death and amputation. Epidemiol Infect. 137:1609–1614.
- Lemsanni M, Najeb Y, Zoukal S, Chafik R, Madhar M, Elhaoury H. (2021). Necrotizing fasciitis of the upper extremity: a retrospective analysis of 19 cases, Hand Surg Rehab. 40(4):505-512.
- Cheng NC, Tai HC, Chang SC, Chang CH, Lai HS. (2015). Necrotizing fasciitis in patients with diabetes mellitus: clinical characteristics and risk factors for mortality. BMC Infect Dis. 15:417.
- Shaikh N. (2007). Necrotizing fasciitis and diabetes mellitus. Int J Diab Dev Ctries.
- Chen PC, Tsai SH, Wang JC, Tzeng YS, Wang YC, Chu CM, et al. (2019). An elevated Glycemic gap predicts adverse outcomes in Diabetic patients with necrotizing fasciitis. PLoS ONE. 14(10):e0223126.
- Tan JH, Koh BT, Hong CC, Lim SH, Liang S, Chan GW, et al. (2016). A comparison of necrotising fasciitis in diabetics and non-diabetics: a review of 127 patients. 98-B(11):1563-1568.
- Oncul O, Erenoglu C, Top C, Küçükardali Y, Karabudak O, Kurt Y, et al. (2008). Necrotizing fasciitis: A life-threatening clinical disorder in uncontrolled type 2 diabetic patients. Diabetes Res Clin Pract. 80:218–223
- Ekka NMP, Kujur ADS, Mishra G. (2019). Necrotizing fasciitis: a tertiary centre based study. Int Surg J. 6:233-238.
- van Stigt S, Knubben M, Schrooten T, Tan E. (2022). Prognostic factors for mortality in 123 severe cases of necrotizing fasciitis in 5 hospitals in the Netherlands between 2003 and 2017. Eur J Trauma Emerg Surg. 48:1189–1195.
- Hillson R. (2023). Unusual infections and diabetes: necrotising fasciitis, practical diabetes. 40.
- Narsingh NP, Nigam A, Kumar R. (2019). A study on role of laboratory risk indicator for necrotizing fasciitis score in necrotizing fasciitis. Int Surg J. 6(11):3901-3905.
- Shivalingappa S, Manjunath KN, Waiker V, Kumaraswamy M, Odeyar U. (2021). Necrotising Fasciitis: Appearances Can Be Deceptive. World J Plast Surg. 10(1):43-52.
- Shukla A, Sharma A. (2017). Clinical study of necrotizing fasciitis and its management. Int Surg J. 4(6):1964-1967.
 Abstract
Abstract  PDF
PDF